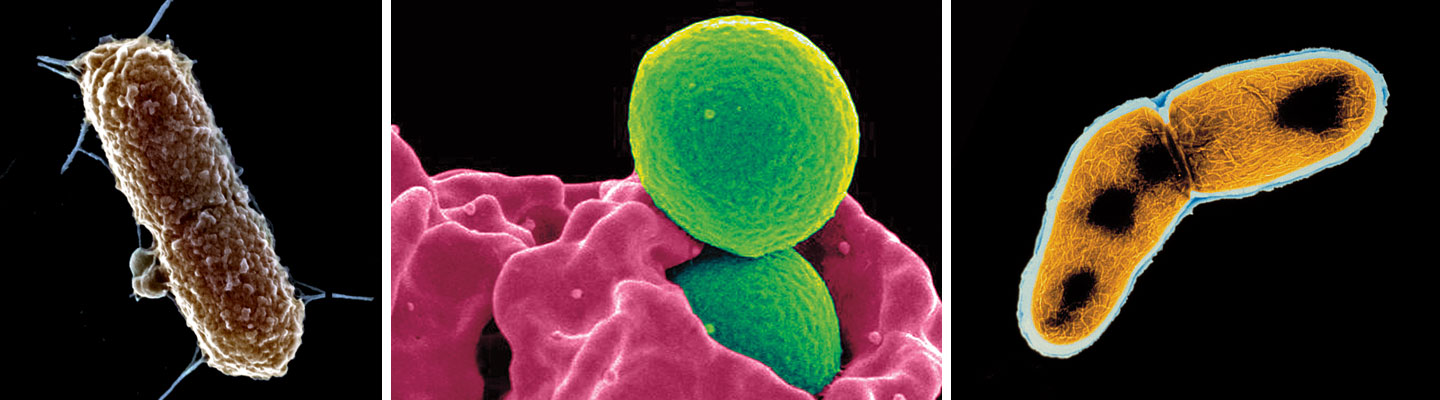
Last April, a woman checked into a medical clinic in Pennsylvania with what appeared to be a routine infection. But doctors soon realized she had something far more serious: a strain of the Escherichia coli, or E. coli, bacterium that was resistant to colistin, one of the most powerful antibiotics. Antibiotics are medications that fight against disease-causing bacteria.
Colistin is a last resort against bacteria that don’t respond to any other type of antibiotic. Luckily, the woman responded to other treatment. But scientists worry that antibiotic resistance is spreading, creating more hard-to-treat bad bacteria known as “superbugs.”
Last April, a woman checked into a medical clinic in Pennsylvania. She had what seemed to be a common infection. But doctors soon found that the problem was far more serious. The microbes making her sick were a rare and dangerous strain of the Escherichia coli, or E. coli bacterium. Doctors use antibiotics to fight these bacteria, but tests turned up bad news. One of the most powerful antibiotics wouldn’t work. The microbes were resistant to it.
This medication, named colistin, is a last resort. Doctors use it against bacteria that don’t respond to any other antibiotic. Luckily, the woman responded to other treatment. But scientists worry that antibiotic resistance is spreading. This creates more hard-to-treat bacteria called “superbugs.”