The Covid-19 pandemic has affected certain groups in the United States—particularly Black, Latine, and Indigenous people—much more than others. According to the U.S. Centers for Disease Control and Prevention (CDC), Indigenous people were nearly four times as likely to be hospitalized and more than twice as likely to die from the virus that causes Covid-19 as White Americans were.
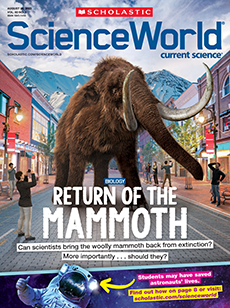
ONLINE EXCLUSIVE
Banding Together
Native American communities were hit hard by Covid-19. Now they’re leading the vaccination effort.
Micah Garen/Getty Images
GETTING VACCINATED: Lance Whitehair (left), a Navajo doctor, and Bijiibaa' Kristin Garrison (right), a Navajo surgeon, received their Covid-19 vaccines at Northern Navajo Medical Center on December 15, 2020 in Shiprock, New Mexico. They were among the first in the Navajo Nation to receive their vaccinations.
Courtesy of Stephanie Carroll Russo
DEALING WITH DATA: Stephanie Russo Carroll’s research explores the links between Indigenous governance, data, the environment, and community wellness.
Vaccines have brought renewed hope to tribal nations, which have been leading efforts to get their citizens vaccinated. The vaccine rollout in Native American communities has prioritized vaccinating elders—people who often hold knowledge of tribal traditions and languages. Because of their age, elders are more vulnerable to developing deadly cases of Covid-19.
Science World spoke with Stephanie Russo Carroll, a professor of public health and American Indian studies at the University of Arizona. Carroll is also an Alaska Native Ahtna woman and a citizen of the Native Village of Kluti-Kaah. She explained why Covid-19 had such a devastating impact on tribal nations and how these communities worked to protect their members during the pandemic.
How has the coronavirus pandemic affected Native communities?
The effects of the pandemic were really magnified in Native communities. There were significant losses of elders, as well as people between the ages of 20 and 50. We all know someone who’s passed away or gotten really sick. That’s the hard part.
Fortunately, tribes and Native health authorities have been able to rely upon the tight social networks and existing ways to deliver health care within their communities to get the vaccine out and slow the spread of Covid-19. As a result, they have done fantastic jobs with the vaccine rollout in ways that you didn’t see anywhere else. By June 2021, the Navajo Nation, a tribe of about 400,000 people in the Southwestern U.S., had fully vaccinated more than 70 percent of its adult population. Around the same time, about 40 percent of the U.S. population had been vaccinated. Many tribes were the first to offer vaccines to all eligible age groups and share with neighboring populations, including people outside tribes.
Why has the pandemic hit these communities so hard?
The U.S. recognizes 574 American Indian tribes and Alaska Native villages as sovereign nations with their own systems of government. These tribes are responsible for maintaining the public health of their members just like the federal government, states, or counties would for its citizens. To accomplish that, the U.S. government is responsible for providing tribes with resources, like public health infrastructure. That allows tribal communities to evaluate, plan, and respond to public health threats like disease outbreaks. It allows tribes to collect data about their members’ health, have access to laboratory testing, and provide medical care. But because the federal government wasn’t investing in the tribes’ public health infrastructure, some tribal health authorities didn’t have the necessary resources, training, or staff to respond to the coronavirus pandemic.
Caravan Images/Alamy Stock Photo
WEATHERING A STORM: The Wupatki Spirit Totem is found at the edge of Navajo land in Flagstaff, Arizona. Its three figures are shown here wearing masks during the Covid-19 pandemic.
Indigenous peoples in the U.S. have suffered a long history of discrimination and oppression, for example, being forced off their ancestral lands and onto distant reservations. In these rural communities there can be limited access to healthy food. As a result, Native people are more likely to suffer from underlying health conditions—like heart disease and diabetes—that can worsen Covid-19. A lot of industrial activity and mining has taken place near Native communities because of their remote locations. These activities can contaminate water supplies and lead to additional health issues.
Have any other factors contributed to the difficulties that Native people experienced during the pandemic?
The federal, state, and local health authorities collect public health data about populations in the U.S. This information helped government authorities make important decisions during the pandemic, like: Should we require people to wear masks? When will we reopen restaurants? Who needs care after hospitalization? But during the pandemic, the CDC and some states wouldn’t share their data with tribes—highlighting coordination issues between tribes and federal and state agencies. According to the CDC, sharing the data was a privacy risk. Meanwhile, this data was being freely shared among the CDC and U.S. state health authorities.
Additionally, many states don’t collect or report detailed information about race or ethnicity in relation to Covid-19 cases. Because of that, the data we did have didn’t reflect how Indigenous people specifically were being affected by Covid-19. That’s a problem. Without data that describes a population accurately, we can’t make life-or-death decisions. For example: Which hospitals need access to important medical equipment, like ventilators?
Can you describe the vaccine rollout in Native communities?
Some tribes have prioritized vaccinating Native language speakers. That’s because when you lose language, you lose culture. Language contains knowledge of ceremonies and traditions. It links us to our roles and responsibilities within communities and strengthens the relationship between people and the land. Language isn’t just words—it also teaches ways of thinking. There are some things you can say in one language but not another.
In many tribal communities, only a small percentage of people are Native language speakers. Nearly all of them are older. Many tribes are in the process of revitalizing Native language, working to introduce online learning for adults and organize preschool programs taught in the Native language.
Noel Lyn Smith/The Daily Times via Imagn Content Services, LLC
PROTECTING A COMMUNITY: An elder from the Navajo Nation receives the Pfizer-BioNTech Covid-19 vaccine in late December at the Gallup Indian Medical Center in New Mexico.
Looking back at how the U.S. colonized, or established political control over, Native American communities, many of the actions that harmed Indigenous peoples broke down the fabric of our society. As well as moving people to reservations far away from their homeland, the government also forcibly removed Native children from their families and placed them in boarding schools. These actions destroyed community bonds. But language can reconnect people. So, when we lose elders with this knowledge, we’re losing part of what holds our communities together. To vaccinate them is to protect our communities. To vaccinate everyone is to protect our peoples.